TABLE OF CONTENTS
Enteritis in Animals
Inflammation of the intestinal mucosa results in diarrhoea, dysentery (faeces mixed with mucus and blood), and accompanying signs of dehydration and acid-base imbalance in animals, which is called enteritis. Occasionally, signs of abdominal pain are also seen.
Etiology
The etiology or causes of enteritis in animals are various bacteria, viruses, parasites, fungi, and chemicals.
Bacteria
- E. coli is commonly associated in calves below 1 week of age.
- Salmonellosis: S. typhimurium and S. Dublin are common in young animals but also seen in adults.
- Cl. perfringens A, B,C, and E are associated with hemorrhagic enteritis.
- M. paratuberculosis causes Johnes disease in adults.
Viruses
- In cattle, BVD, malignant catarrh, and RP cause enteritis.
- In young ones, the Rota and Corona viruses cause enteritis.
- In dogs, Corona, Parvo, CD, and ICH cause enteritis.
- In piglets, TGE causes enteritis.
- In adult pigs, hog cholera (swine fever) causes enteritis.
Parasites
Majority of nematodes and cestodes cause enteritis:
Nematodes
- Nematodes: Toxocara vitullorum
- Young calves: Strongyles-trichostrongyles, Bunostomum<Haemonchus, Trichuris spp.
- Dogs and Cats: Toxocara canis, T. cati, Ancylostoma caninum, and Toxocaris leonine.
- Flukes/trematodes: immature amphistomes are normally associated.
Cestodes
- Cattle and sheep: Monezia expansa, M. benedini
- Equines: Anaplocephala magna
- Dogs: Dipyllidium caninum, Diphylobothrium latum, etc.
Protozoa
- Coccidiosis: Eimeria and Isospora.
- Cryptosporidia parvum causes enteritis in young calves (1 month of age showing recurrent diarrhoea should be thoroughly screened for cryptosporidiosis).
- Chlamydial spp., like Chlamydia psittacii, cause enteritis.
Fungi
Candida and Aspergillus spp. cause enteritis in animals on prolonged oral antibiotic therapy and are likely to develop fungal enteritis.
Chemicals
Pb (lead), Mb (molybdenum), Nitrate,Nitrate Cu (copper), As (arsenic), and also Hg (mercury) cause enteritis in animals. Managemental conditions like poor nutrition, poor ventilation, and poor hygiene also cause enteritis.
Pathogenesis
Inflammation of the gastrointestinal mucosa causes a failure of absorption that leads to diarrhea. The mechanism of diarrhoea is categorised into four types:
- Osmotic diarrhoea
- Secretary diarrhoea
- Exudative type of diarrhoea
- Diarrhoea due to abnormal motility or decreased transit time
Osmotic diarrhoea
Osmotic diarrhoea occurs mainly because of decreased absorption from the gut, leading to increased osmolarity of the intestinal content, and there is overdistention, resulting in diarrhoea.
Osmotic diarrhoea in lactose intolerance: lactose is not digested, and this will be utilised by some microflora and converted into organic acid, causing an increase in osmolarity, leading to overdistention and iarrhea. This is also possible in other conditions where the absorptive surface decreases. Eg-TGE in piglets, rotavirus/coronavirus enteritis in calves, and a dog cause selective destruction of the villus surface of absorptive cells.
Secretary diarrhoea
In secretary diarrhoea, mechanisms stimulate the intestinal mucous to secrete more fluid in the lumen, and therefore the rate of secretion exceeds absorption. The best example of this is the entero-toxigenic strains of E. coli. Increased secretion is due to stimulation of PG synthesis.
Exudative type of diarrhoea
The mucosal permeability is changed to such an extent that there is increased trans-mucosal hydrostatic pressure, resulting in a net loss of protein and fluid in the lumen. Usually, third-degree damage to the gut mucosa results in this type, which is often known as protein losing enteropathy. Examples are lymphatic enteritis, eosinophilic enteritis .
Diarrhoea due to abnormal motility or decreased transit time
Hypermotility due to increased peristalsis results in recurrent evacuation of the bowel, and here there is less time for digestion and assimilation. Increased transit time favours bacterial overgrowth.
- SIBO: Small intestinal bacterial overload or overgrowth is a common cause of this type of diarrhoea.
- IBD, or inflammatory bowel disease, is also responsible for hypermotility.
- In acute diarrhoea, fluid and electrolyte loss is their decreased absorption responsible for the net loss of weight. Chronic episodes result in debilitating types of diarrhoea, like Johnes disease.
Major biochemical changes in Enteritis
Enteritis in animals leads to diarrhoea, which leads to these biochemical changes:
- Metabolic acidosis due to net bicarbonate loss
- Loss of fluid cause dehydration
- Hyponatremia and hypokalemia
In chronic entropathies, the net loss of protein leads to hypoproteinemia, and therefore animals with chronic diarrhoea show signs of wasting. E.g., Johns disease and parasitic enteritis.
Hypoproteinemia leads to decreased colloidal osmotic pressure in plasma, and fluid accumulates in body spaces. e.g., bottle jaw.
Clinical Signs
- Clinical signs vary depending on whether it is an acute or chronic form of enteritis.
- Diarrhoea: it may be alone or with mucous and blood in dysentery.
- Depending on contributory factors, other systemic signs are seen, like fever, anorexia, signs of toxaemia, septicemia, and signs of dehydration.
Following are few characteristics of changes in the faeces of animals:
- Colibacillosis of young calves: a chalky white type of diarrhea.
- Parvo-viral and corona viral disease: foul smelling brown coloured faeces, sometimes mucous shreds.
- Pancake like stool is seen in CPV gastroenteritis.
- Shooting type of diarrhoea in RP.
- Varying degrees of dehydration is common in acute diarrhoea.
Diagnosis
Differences are shown in a table below for small bowel diarrhoea and large bowel diarrhoea:
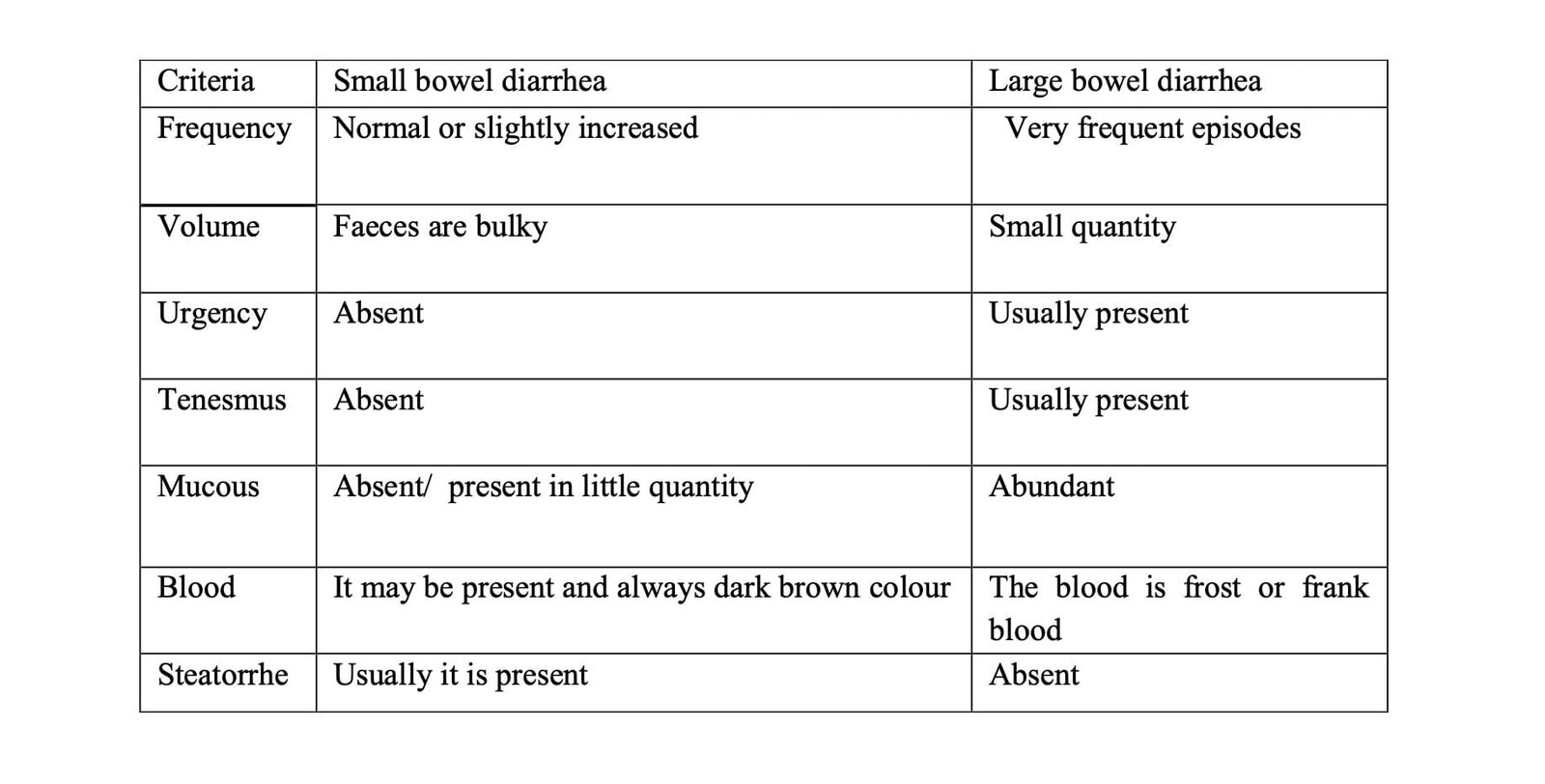
Generally, vomiting is present in small bowel diarrhoea but absent in large bowel diarrhoea.
Examination of faeces for diagnosis
Microscopic examination: parasitic ova or cysts are identified in parasitic enteritis when the faecal smear is negative, which may be due to bacterial or viral disease.
- Bacterial enteritis: go for culture and sensitivity testing.
- Viral enteritis: go for serology (HA and HI are commonest).
Biochemical parameters for diagnosis
- Plasma protein estimation also helps in the diagnosis of chronic enteritis (hypoprotenemia).
- Bicarbonate, blood pH, sodium, potassium, PCV, and total serum solid estimation are helpful to confirm acid-base disturbance and the amount of dehydration.
- Usually, leucopenia suggests viral involvement as a primary or secondary complication.
Treatment
The principles of treatment for enteritis in animals are:
- Removal of the primary cause, identification of the causative agent, and its removal.
- Replacement of the fluid and electrolyte.
- Stabilising the GI motility.
In parasitic eneteritis, antiparasitic medications are given, like niclosemide 75–150 mg/kg body weight and praziquantel 5 mg/kg body weight PO in the case of Cestode. Closantel at 7.5 mg/kg body weight and oxyclozanide at 15-20 mg/kg PO in the case of Trematodes.
Preferably, an antibiotic course is practiced to prevent secondary infection in viral enteritis; a parenteral route is preferred.
Enrofloxacin , gentamicin , amoxicillin+cloxacillin, and cefotaxime are used in canine parvo viral GE.
Protozoal and bacterial enteritis in bovines can be treated with gut acting antibacterials like sulphonamides, furazolidone, and a combination of metronidazole and furazolidone.
Stabilizing GI motility
Loperamide tablets are used in dogs; 1/2 to 1 tab TID, reduces peristalsis and prevents recurrent evacuation of the bowel, but in acute diarrhoea, loperamide is not advised.
GI protectant astringents and smoothening agents like kaolin, pectin have very good effects. They inhibit secretion from the mucosa by coating the mucosa, and they increase solids in the faeces by helping to form the stool. For large animals, commercial antidiarrheal or astringents are available, which help precipitate proteins, solidify faeces, and soothe the GIT. For examples, Neblon powder, diaspel powder, and diaroak powder are given at 40–60 gm, BID PO, for 3-5 days.
Oral administration of probiotics helps in the rejuvenation of the intestinal microflora. lactobacillus given orally (sporolac) to control the enteritis.

