TABLE OF CONTENTS
Monday Morning Sickness in Horses
Monday Morning Sickness in Horses in horses is a syndrome of muscle fatigue, pain, or cramping associated with exercise. Less common exertional myopathies that cause exercise intolerance without muscle necrosis include mitochondrial myopathies and forms of polysaccharide storage myopathy in Warmblood horses.
Monday Morning Sickness in Horses also known as Exertional myopathy and Exertional Rhabdomyolysis (ER).
Most commonly, exertional myopathies produce necrosis of striated skeletal muscle and are termed exertional rhabdomyolysis. Although exertional rhabdomyolysis was previously considered a single disease described as azoturia, tying-up, or cording up, it is now known to comprise several different myopathies, which, despite similarities in clinical presentation, differ significantly in etiopathology.
Etiology
Beyond a highly probable hereditary factor, there does not seem to be a single cause that triggers ER in horses. Exercise is seen in every case, but exercise is always accompanied by another factor. It is likely that several factors must act together in order to cause an ER attack.
Other possible factors include–
- The overfeeding of non-structural carbohydrates (grain and pellets, for example)
- Poor conditioning or fitness, sudden increase of workload
- The work of a horse after a period of rest, if the concentrate ration was not reduced
- Electrolyte or mineral imbalances, especially seen with potassium
- A deficiency in selenium or vitamin E
- Imbalance of hormones, including the reproductive hormones in nervous fillies and mares and thyroid hormones in horses with hypothyroidism
- Wet, cold, or windy weather conditions
The more factors that are present, the greater the likelihood that the horse will develop ER. However, the most common cause of ER is an imbalance between the animal’s diet and his workload, especially when he has a high-grain diet.
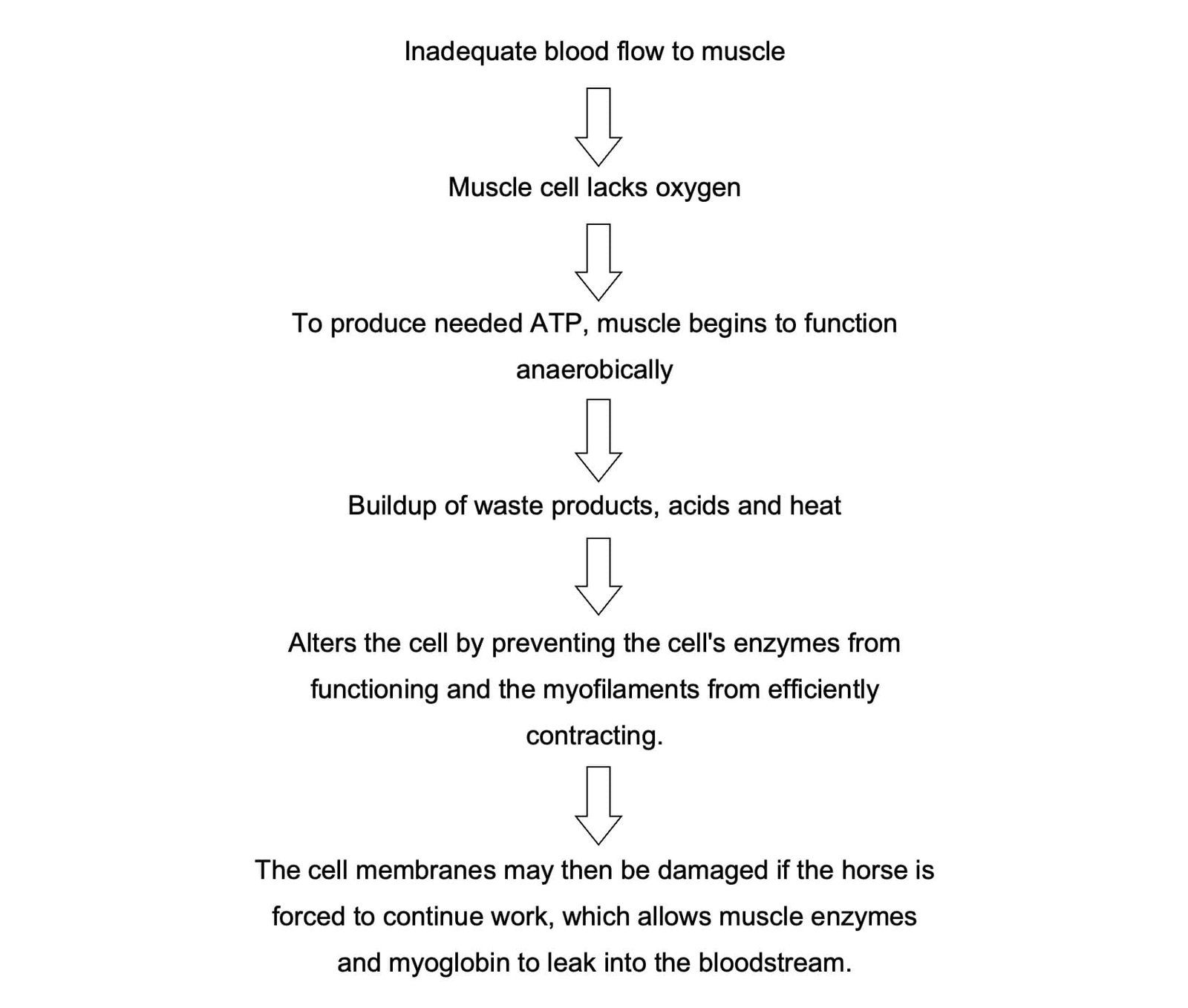
The body builds up a store of glycogen from converted carbohydrates in muscle cells. Glycogen, a fuel used by muscles for energy, is depleted during work and restocked when a horse rests. Oxygen-carrying blood metabolizes glycogen, but the blood can not flow fast enough to metabolise the excess stored glycogen. The glycogen that is not metabolized aerobically (by the oxygenated blood) must then be metabolized anaerobically, which then creates the cell waste products and heat, and ER has begun. A horse on a high-grain diet with little work collects more glycogen in its muscles than it can use efficiently when exercise begins, which is why horses on a high-grain diet are more likely to develop ER.
Proper conditioning can help prevent Monday Morning Sickness in Horses, as it promotes the growth of capillaries in muscles and the number of enzymes used for energy production in muscle cells. However, improvement in these areas can take several weeks. Thus, ER is more common in horses that are only worked sporadically or lightly, and in horses just beginning an exercise regimen.
A common misconception is that Monday Morning Sickness in Horses is caused by the buildup of lactic acid. Lactate is not a waste product for a cell, but a fuel, used when the cell’s oxygen supply is insufficient. Lactate does not damage a cell, but is rather a byproduct of the true cause of cell damage: inadequate blood supply and altered cell function. Lactate naturally builds up in an exercising horse without harming the muscle cells, and is metabolized within an hour afterward.
The pain is caused by the inadequate blood flow to the muscle tissue, the inflammation from the resulting cell damage, and the release of cell contents. Muscle spasms, caused by the lack of blood to the muscle tissue, are also painful.
Clinical signs usually are seen shortly after onset of exercise–
- Excessive sweating,
- Tachypnea,
- Tachycardia,
- Muscle fasciculations,
- Reluctance or refusal to move, and
- Firm, painful lumbar and gluteal musculature are common signs.
Episodes range from subclinical to severe muscle necrosis with recumbency and myoglobinuric renal failure. The severity varies extensively between individuals and to some degree within the same individual. A diagnosis of exertional rhabdomyolysis is based on demonstration of abnormal increases in serum CK, lactate dehydrogenase, and AST.
Exertional rhabdomyolysis can be either sporadic, with single or very infrequent episodes of exercise-induced muscle necrosis, or chronic, with repeated episodes of rhabdomyolysis and increased serum CK or AST with mild exertion.
SPORADIC EXERTIONAL RHABDOMYOLYSIS
All breeds of horses are susceptible to sporadic exertional rhabdomyolysis. The most common cause is exercise that exceeds the horse’s state of training. The incidence of muscle stiffness also has been found to increase during an outbreak of respiratory disease. Dietary deficiencies of sodium, vitamin E, selenium, or a calcium:phosphorus imbalance may also be contributory factors.
A diagnosis of sporadic exertional rhabdomyolysis is made on the basis of a horse with no previous history, or a brief history, of exertional rhabdomyolysis, signs of muscle cramping and stiffness after exercise, and moderate to marked increases in serum CK and AST. Immediately on detection of signs of exertional rhabdomyolysis, exercise should stop and the horse should be moved to a well-bedded stall with access to fresh water. The objectives of treatment are to relieve anxiety and muscle pain and to correct fluid and acid-base deficits. Tranquilizers or opioids may be given. NSAIDs can be given to a well-hydrated horse. Most horses are relatively pain free within 18–24 hr.
Severe rhabdomyolysis can lead to renal compromise due to ischemia and the combined nephrotoxic effects of myoglobinuria, dehydration, and NSAID therapy. The first priority in horses with hemoconcentration or myoglobinuria is to reestablish fluid balance and induce diuresis. In severely affected animals, regular monitoring of BUN and/or serum creatinine is advised to assess the extent of renal damage. Diuretics are contraindicated in the absence of IV fluid therapy and are indicated if the horse is in oliguric renal failure.
Horses should be stall rested on a hay diet with a dietary vitamin and mineral ration balancer supplement for a few days. For horses with sporadic forms of exertional rhabdomyolysis, rest with regular access to a paddock should continue until serum muscle enzyme concentrations are normal. Because the inciting cause is usually temporary, most horses respond to rest, a gradual increase in training, and dietary adjustment. Endurance horses should be encouraged to drink electrolyte-supplemented water during an endurance ride and monitored particularly closely during hot, humid conditions.
CHRONIC EXERTIONAL RHABDOMYOLYSIS
Some horses have recurrent episodes of rhabdomyolysis, even with light exercise. Four forms of chronic tying-up have been identified using muscle biopsies or genetic testing:
- Type 1 polysaccharide storage myopathy (PSSM),
- Type 2 PSSM,
- Malignant hyperthermia
- Recurrent exertional rhabdomyolysis.
Type 1 polysaccharide storage myopathy
Type 1 polysaccharide storage myopathy is seen frequently in Quarter horse–related breeds (especially halter and Western pleasure horses), Morgans, and draft horses but is also present in at least 20 other horse breeds. It is caused by a dominantly inherited mutation in the glycogen synthase 1 (GYS1) gene. A diagnosis can be made by genetic testing of blood or hair samples. Quarter horse–related breeds and other crossbred or light breeds of horses with type 1 PSSM often develop episodes of rhabdomyolysis at a young age with little exercise. Rest for a few days before exercise is a common triggering factor. Episodes are characterized by a tucked-up abdomen, a camped-out stance, muscle fasciculations, sweating, gait asymmetry, hindlimb stiffness, and reluctance to move. Some horses paw or roll, resembling equine colic.
Type 2 polysaccharide storage myopathy
Type 2 polysaccharide storage myopathy occurs in light breeds such as Arabians, Morgans, Thoroughbreds, a variety of Warmblood breeds and some Quarter horses. A diagnosis is made by identifying an abnormal pattern of glycogen storage in muscle biopsies in a horse with a negative GYS1 genetic test. In Quarter horses <1 yr old, it may cause difficulty rising from a recumbent position and increased serum CK activity. Chronic episodes of muscle stiffness, soreness, and muscle atrophy with normal to modest increases in serum CK are common in horses with type 2 PSSM. The most common presentation of this disorder in Warmbloods is a gait abnormality, exercise intolerance, and loss of muscle mass when out of work that is not necessarily accompanied by a concomitant rise in serum CK.
Malignant hyperthermia
Malignant hyperthermia is caused by an autosomal dominant mutation in the skeletal muscle ryanodine receptor gene (RYR1). The mutation is responsible for both anesthesia-related and non-anesthesia-related causes of rhabdomyolysis in Quarter horses. A diagnosis can be made by genetic testing of blood or hair roots. Signs related to inhalation anaesthesia include tachycardia, tachypnea, hyperthermia, muscle rigidity accompanied by a severe lactic acidosis, increased serum CK, and electrolyte derangements. Exertional rhabdomyolysis in Quarter horses with malignant hyperthermia can result in sudden death. Signs are preceded by excessive sweating, tachycardia, tachypnea, hyperthermia, and muscle rigidity. Some Quarter horses have both malignant hyperthermia and PSSM, which results in more severe signs of exertional rhabdomyolysis than those seen in horses with PSSM alone.
Recurrent exertional rabdomyolysis
Recurrent exertional rabdomyolysis is seen frequently in Thoroughbreds, Standardbreds, and Arabian horses. It is likely due to abnormal regulation of intracellular calcium in skeletal muscles. It appears there is intermittent disruption of muscle contraction, particularly when horses susceptible to the condition are fit and have a nervous temperament. In Thoroughbreds, it is likely inherited as an autosomal dominant trait.
Diagnosis
Diagnostic tests to determine the cause of chronic tying-up include a CBC, serum chemistry panel, serum vitamin E and selenium concentrations, urinalysis to determine electrolyte balance, dietary analysis, exercise testing, muscle biopsy, and genetic testing. An exercise challenge test is useful to detect subclinical cases; serum CK is measured before and 4 hr after light exercise. In addition, quantifying the extent of exertional rhabdomyolysis during mild exercise is helpful in deciding how rapidly to reinstate training.
Treatment
Horses with type 1 PSSM have constitutively active glycogen synthase that is further stimulated by increased blood insulin concentrations, resulting in high muscle glycogen concentrations. When fed a starch meal, these horses take up a higher proportion of the absorbed glucose in their muscles than healthy horses. Horses with type 2 PSSM also have abnormal glycogen storage, but the cause of this myopathy is unknown. Thus, the ideal diet for PSSM is based on feeding forage at a rate of 1.5%–2% body wt, providing >15% of digestible energy as fat and limiting starch to <10% of daily digestible energy by limiting grain or replacing it with a fat supplement. Caloric needs should be assessed first to prevent horses becoming obese on a high-fat diet. Improvement in signs of exertional rhabdomyolysis for horses with PSSM requires both dietary changes and gradual increases in the amount of daily exercise and turn-out.
Horses with malignant hyperthermia may benefit from premedication with dantrolene (4 mg/kg, PO) 60–90 min before exercise, particularly under hot conditions.
Dantrolene (4 mg/kg, PO) given 1 hr before exercise may decrease the release of calcium from the calcium release channel. Phenytoin (1.4–2.7 mg/kg, PO, bid) has also been advocated as a treatment for horses with recurrent exertional rhabdomyolysis. Therapeutic levels vary, so oral dosages are adjusted by monitoring serum levels to achieve 8–12 mcg/mL. However, longterm treatment with dantrolene or phenytoin is expensive.