TABLE OF CONTENTS
Ring bone in horses
Ring bone in horses is the exostosis on the phalangeal bone. Typical ringbone is an osteo-arthritis involving the inter-phalangeal joints.
Ring bone in horses is classified as true ring bone and false ring bone. In true ring bone the exostosis is at interphalangeal joints. A false ring bone is an exostosis on the shaft of phalangeal bone.
Ring bone also classified as high ring bone and low ring bone. The term “high ringbone” is often used synonymously with OA (Osteoarthritis) of the PIP (Proximal Inter Phalangeal) joint. Historically ringbone has been used to describe any bony enlargement of the phalanges in the pastern region below the fetlock joint. If the bony enlargement was associated with the distal aspect of P1 and proximal aspect of P2 with or without PIP joint involvement it was classified as high ringbone. If the bony enlargement was associated with the distal aspect of P2 and the proximal aspect of the distal phalanx with or without distal interphalangeal (DIP) joint involvement it was classified as low ringbone.
Ringbone has also been classified as articular (involving the joint surface) or periarticular (involving the structures at the perimeter of the joint and the adjacent phalanges).
Etiology
- Hereditary predisposition
- Defective confirmation
- Poor quality of bone
- Uneven weight bearing due to improper shoeing
- Use of calkins
- Rickets
- Direct trauma
- Concussion
- Sprain of articular ligaments
- Fissure fracture of os-suffraginis or os-corona
Clinical signs
- Osteo-periostitis with pain and lameness until exostosis develops
- Focal or diffuse enlargement
- Exostosis cause mechanical interference by the opposite foot during progression
- Articular ring bone cause severe lameness
- Lameness may be more pronounced during trot and is more uphill
- Periarticular ringbone is more commonly seen on the lateral aspect of saffragio-coronal joint and may not cause lameness.
- Low ring bone whether articular or periarticular cause lameness because of the pain caused by pressure exerted within the hoof
- In low ring bone a hard, bony swelling may be noted in the region of coronet

Diagnosis
- Based on clinical signs
- Diagnostic nerve block
- Radiography
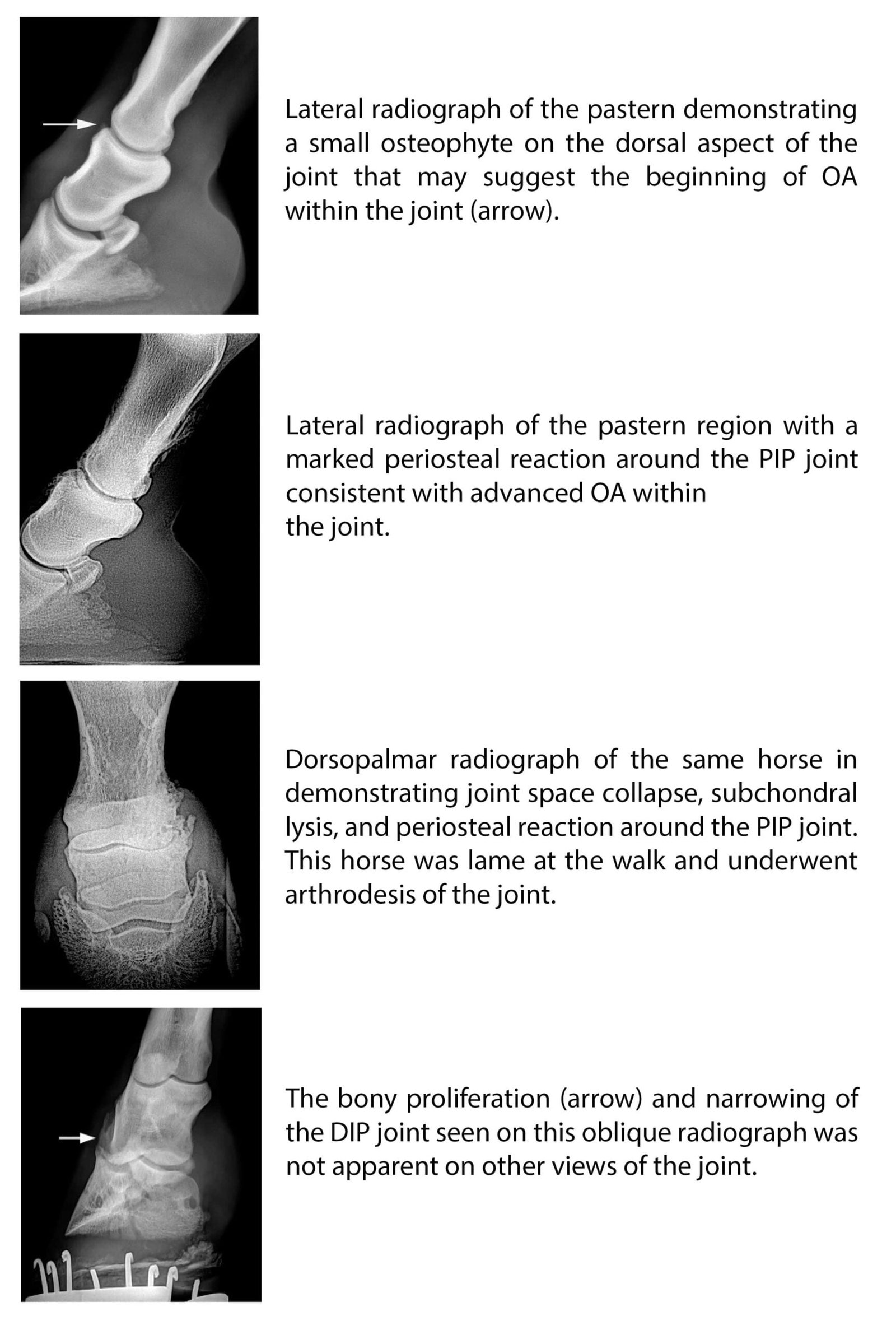
- (1) joint space narrowing or collapse
- (2) osteophyte formation
- (3) subchondral bone sclerosis
- (4) periosteal/periarticular bony proliferation
- (5) deformity/collapse of the joint space
- Other radiographic features that may be identified include subchondral bone lysis, subchondral cystic lesions and chronic eminence fractures of P2.
Treatment
- Rest in acute stage
- Blistering and needle point firing
- Neurectomy of both plantar nerve is advisible to make the animal useful for work
- Low ring bone
- Inter articular medication and corrective shoeing
- Direct medication of DIP using corticosteroids alone or with HA or PSGAG
- High ring bone
- Hoof trimming and therapeutic shoeing
- NSAID – phenyl butazone, Flunixin meglumine along with bandaging
- For chronic cases, NSAIDs can be given prior to, during the days of performance, and for 1 to 2 days after performance to permit some horses to perform relatively pain free for prolonged periods.
- Intermittent use of phenylbutazone for a few days at a time is thought to reduce the complications that may be associated with prolonged,continuous use of the drug.
- Oral NSAID with IA corticosteroids and HA
- A combination of a steroid (triamcinolone or methylprednisolone acetate) and hyaluronan (HA) can also be used IA in horses with acute disease to reduce inflammation and slow the progression of the disease.
- Intramuscularly or IA polysulfated glycosaminoglycans (PSGAGs), IV HA, and oral nutraceutical supplements may be used concurrently but appear to be most beneficial in horses with mild to moderate OA of the PIP joint.
- Surgical treatment for OA of the PIP joint consists of arthrodesis, which is aimed at eliminating motion within the joint, thereby decreasing pain and lameness.
- Natural ankylosis of the PIP joint may occur, but it is often a long, painful process with variable results.
- Surgical arthrodesis is generally considered a better solution with more consistent results.
- The basic principles include removal of the articular cartilage; internal fixation of P1 and P2 with screws, plates, or a combination of plates and screws; compression across the joint surface; accurate alignment of the phalanges; and variable periods of external immobilization with a half-limb cast.
- Current recommended techniques include a single dorsal midline plate with 2 additional transarticular 4.5- or 5.5-mm screws, or 2 dorsally applied plates with or without transarticular screws.
- Dynamic compression plates (DCP), limited contact dynamic compression plates(LC-DCP), and locking compression plates (LCP) may be used.
- After surgery the limb is usually immobilized in a lower limb fiberglass cast (just below the carpus or tarsus and incorporating the foot).
- However, horses that had a PIP joint arthrodesis performed with a minimally invasive procedure were only placed in a bandage and splint after surgery.
- After the cast or bandage and splint are removed stall confinement is recommended for at least another 6 to 8 weeks. Increasing periods of hand-walking exercise can usually begin during this time.
- Although some horses may be ready to return to performance by 6 months, up to a year of convalescence may be required for others.
- In general, the prognosis for horses following PIP joint arthrodesis is less predictable in the forelimb than in the hindlimb.
- After arthrodesis of the PIP joint, approximately 89% to 95% of horses with hindlimb and 70% to 85% of horses with forelimb lameness should return to their intended use.