TABLE OF CONTENTS
Inhalant Anaesthetics
Inhalant anesthetics in animals are delivered in the respiratory system by use of Anaesthetic machine to induce general anaesthesia.
Inhalent anaesthesia classified as gases and volatile liquids. Based on their use, they are also classified as follows-
- Group I – Agents in current clinical use
- Major use – Halothane, Isoflurane
- Minor use – Enflurane, methoxyflurane, nitrous oxide, ether
- Group II – New agents – Desflurane, sevoflurane
- Group IIIAgents of historical interest
- Chloroform, cyclopropane, fluroxene, trichloroethylene
Properties influencing drug kinetics of inhalant anaesthetics
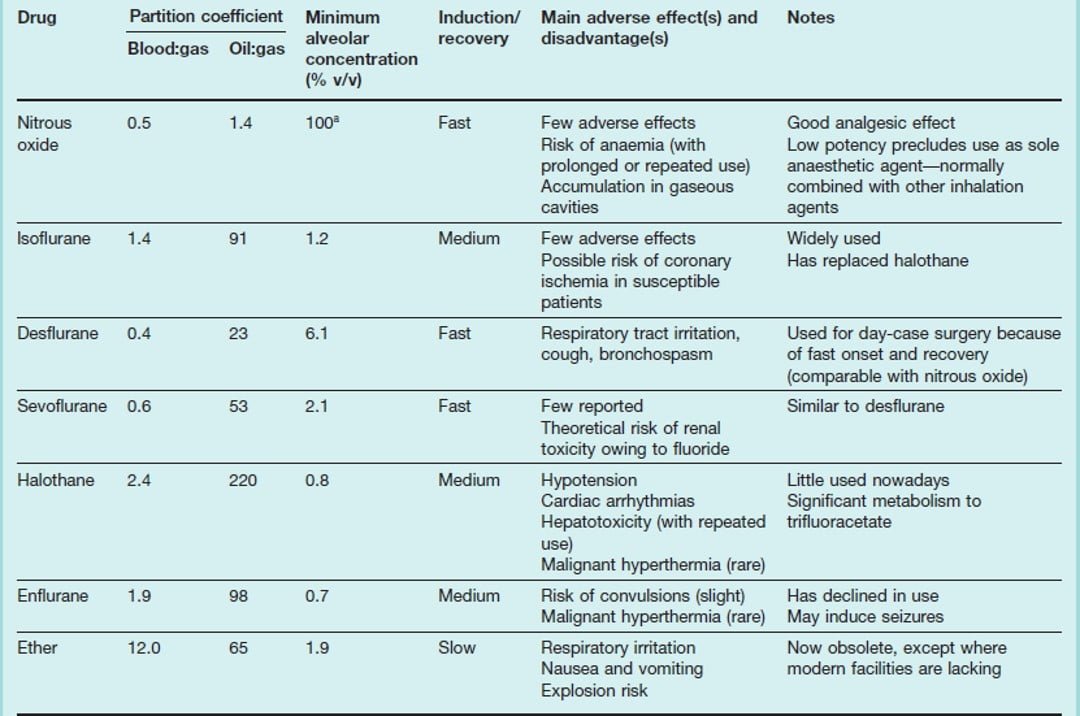
- Solubility – The solubility of an inhalation anesthetic in blood and tissues is characterized by its partition coefficient. An anesthetic agent with a low blood/gas partition coefficient is usually more desirable than a soluble agent because it is associated with (i) a more rapid anesthetic induction, (ii) more precise control of anesthetic depth (iii) more rapid elimination of anesthetic and recovery from anesthesia.
- Blood/gas partition coefficient: This is a measure of the speed of anesthetic induction, recovery and change of anesthetic levels.
- Oil/gas partition coefficient: This describes the ratio of concentration of an anesthetic in oil and gas phases at equilibrium. The oil/gas partition coefficient correlates inversely with anesthetic potency and describes the capacity of lipids for anesthetics.
Pharmacokinetics of inhalant anaesthetics
- Uptake and elimination of inhalation anesthetics – The aim of administering an inhalation anesthetic to a patient is to achieve an adequate partial pressure or tension of anesthetic in the brain, to cause a desired level of anesthesia. Gases move from regions of higher tension to those of lower tension, until equilibrium is established.
- Delivery to the alveoli – This depends on the inspired anesthetic concentration and the magnitude of alveolar ventilation.
- Inspired concentration – The upper limit of inspired concentration is directed by the vapor pressure of the agent that in turn is dependent on the temperature.
- Alveolar ventilation – An increase in alveolar ventilation increases the rate of delivery of inhalation anesthetics to the alveoli. Alveolar ventilation is altered by changes in anesthetic depth, mechanical ventilation or changes in dead space ventilation.
- Removal from alveoli – This is dependent upon the uptake by blood.
- Uptake by blood – Anesthetic uptake is the product of three factors namely (a) solubility, (b) cardiac output and (c) the differences in anesthetic partial pressure between the alveoli and venous blood returning to the lungs.
- Cardiac output – The greater the cardiac output, the more blood passing through the lungs carrying away the anesthetic from the alveoli.
- Alveolar to venous anesthetic partial pressure– The magnitude of difference in anesthetic partial pressure between the alveoli and the venous blood is related to the amount of uptake of anesthetic agent by tissues. The largest gradient occurs during induction.
- Anesthetic recovery – Recovery from inhalation anesthesia results from the elimination of anesthetic from the brain. A factor that is important in the rate of recovery but not during the induction period is the duration of anesthesia. Other factors that are important to varying but smaller degree to inhalation anesthetic elimination from the body include percutaneous loss and inter tissue diffusion of agents.
- Biotransformation – Inhalation anesthetics are not chemically inert. They undergo varying degree of metabolism primarily in the liver, but to a lower degree in the lung, kidney and intestinal tract.
- Anesthetic dose – MAC (minimal alveolar concentration) – Minimal alveolar concentration is the lowest concentration of the anesthetic in pulmonary alveoli needed to produce immobility in response to painful stimulus in 50% of individuals. The MAC of a number of general anesthetics exhibits excellent correlations with their oil/gas partition coefficient. The anesthetic potency of an inhaled anesthetic is inversely related to MAC. Thus, a very potent anesthetic has a low MAC value and a high oil/gas partition coefficient.
| Species | Enflurane | Methoxyflurane | Halothane | Isoflurane | Desflurane | Sevoflurane | Nitrous oxide |
| Cat | 1.2 | 0.23 | 1.14 | 1.63 | 9.8 | 2.58 | 255 |
| Dog | 2.06-2.2 | 0.23 | 0.87 | 1.28 | 7.2 | 2.1-2.36 | 188-297 |
| Horse | 2.12 | 2.8 | 0.88 | 1.31 | 7.6 | 2.31 | 205 |
| Swine | – | – | 0.91 | 2.04 | 10.0 | 2.66 | 162-277 |
| Duck | – | – | 1.03 | 1.30 | – | – | – |
| Rabbit | – | – | 0.82 | – | 8.9 | 3.7 | – |
| Monkey | – | – | 0.89 | – | – | – | 200 |
| Rat | – | 0.27 | 1.11-1.17 | 1.38 | 5.7-7.1 | 2.45 | 136-255 |
Inhalant Anaesthetic drugs
Halothane
- Multihalogenated ethane – introduced in 1957
- Rapid induction, recovery, minimal side effects and nonflammability
- About 20 % metabolized – MAC 0.85% – not irritating to the mucous memb.
- Depresses CNS in a dose related fashion – cerebral blood flow may increase → higher CSF pressure. Shivering found during recovery
- Depression of cardiac output and bradycardia – due to vagus activity
- May sensitize the heart to catecholamines → arrhythmia
- Depresses Minimal neuromuscular blockade and analgesia
- Minimal pathological changes in the liver. Hepatitis may be caused. Some metabolites may cause necrosis
- Kidney unaffected but sometimes as a sequelae to blood flow changes
- Poor muscle relaxation.
- Malignant hyperthermia in pigs and man. Also in other sp.
Isoflurane
- Popular agent.
- MAC – for induction 3-5% and for maintenance – 1.5 – 2.5%
- Flourinated ether. 1% metabolized into fluoride. But not toxic.
- Lesser vasodilatation of the brain. Affects cardiac output less than halothane and has a wider margin of safety.
- Dose dependent depression of the heart and respiration
- Arrhythmias not reported
- Renal function not affected
- Better muscle relaxation than halothane
- Not to be used in animals with a known susceptibility to malignant hyperthermia
- Used in reptiles
- Yet to replace halothane in popularity
Enflurane
- Since 1963
- cardiac depression, decrease cardiac output, decrease arterial BP as good as or higher than halothane
- sensitization of the heart to catecholamines – very mild
- 2-8% metabolized but may not cause fluoride nephrosis.
- Hepatitis reported
Desflurane
- Highly stable – stable at room temp. for > a year
- Boils at close to room temp. and careful vaporization needed
- Low solubility in blood → rapid induction
- 0.2% metabolised
- Not popular in humans because of its irritant nature
- Tendency to cause malignant hyperthermia
Methoxyflurane
- Stable compound
- Less prone to cardiac depression, not irritating
- Polyuric renal dysfunction due to fluoride metabolites
- Hence withdrawn
Ether (diethyl ether)
- Colourless volatile liquid. Stored in a cool place but not in refrigerator
- Inflammable – High blood – gas solubility
- Locally refrigerant, anaesthetic, rubefacient, skin antiseptic
- Nausea and vomition during inhalation — disadvantageous
- Metabolites non toxic
- CNS – slow and unpleasant induction—
- Heart rate and BP decrease due to epinephrine release during induction
- Respiration – Irritant to passage, bronchial and pulmonary complications seen
- Transient depression of liver and kidney – causes metabolic acidosis
- However ether has been in use for more than 100 years
- Classical stages of anaesthesia can be produced
Chloroform
- Unpleasant odour – Powerful rapid inducer
- Sensitizes myocardium to adrenaline → ventricular fibrillation → sudden death (20 – 30 times more potent than ether)
- Toxicity to liver – necrosis, fatty degeneration
- Kidney – anuria
- Poisoning → acidosis, vomiting, acetonuria, albuminuria, pyrexia, icterus,
- Discontinued
Nitrous oxide
- Colorless gas – kept compressed at 40 atm.
- N2O increases pulmonary ventilation – due to direct stimulation of respiration.
- Increases its own inhalation – (Concentration effect)
- and also that of halothane or enflurane or oxygen when given together (second gas effect)
- MAC > 100% (104 in man to 255 in cat) – weak anaesthetic-
- But strongly analgesic
- An anaesthetic adjuvant