Inflammation of the intertubercular bursa
Inflammation of the intertubercular bursa is also known as bicipitalbursitis.
Inflammation of the intertubercular (bicipital) bursa as a primary cause of lameness is uncommon, even though the condition can occur in horses of any age, breed, or sex. It can present as septic or nonseptic.
The bicipital bursa is located between the bilobed tendon of the origin of biceps brachii muscle and the M-shaped tubercles at the cranioproximal aspect of the humerus. The synovial membrane of the bursa extends around the axial and abaxial limits of the tendon and onto the margins of its cranial surface. Although uncommon, communication can exist between the shoulder joint and the bicipital bursa.
Etiology
Trauma to the cranial surface of the shoulder region is believed to be the most common cause of a primary bursitis
Other suggested causes include stretching or tearing of the bursa or biceps tendon during the cranial phase of the stride with the limb in full extension or by a fall or slip that results in flexion of the shoulder with extension of the elbow.
Inflammation of this bursa can also be caused by dislocation of the biceps brachii tendon that may be associated with congenital abnormality of hypoplasia of the minor tubercle.
Infection, either from an open or penetrating wound or from hematogenous spread to the bursa has also been reported.
Brucella abortus, influenza or other viral respiratory diseases also cause bicipitalbursitis.
Clinical Signs
A history of trauma to the shoulder region is the most common factor; the signs of lameness usually have an acute onset which is most obvious during the stance and swing phases of the stride.
On physical examination swelling over the cranial aspect of the shoulder region may be evident with or without a wound being present.
Generalized shoulder and pectoral muscle atrophy may be seen in more chronic cases.
Pressure applied over the biceps tendon and bursal region and manipulation of the shoulder region in flexion and extension usually result in a prominent painful response.
The lameness is often characterized by a shortened cranial phase of the stride, a decrease in the height of the foot flight arc, reduced carpal flexion, and a fixed shoulder appearance during movement.
The horse is often reluctant to bear full weight on the affected limb while standing
Diagnosis
- Shoulder radiograph
- Ultrasound examination
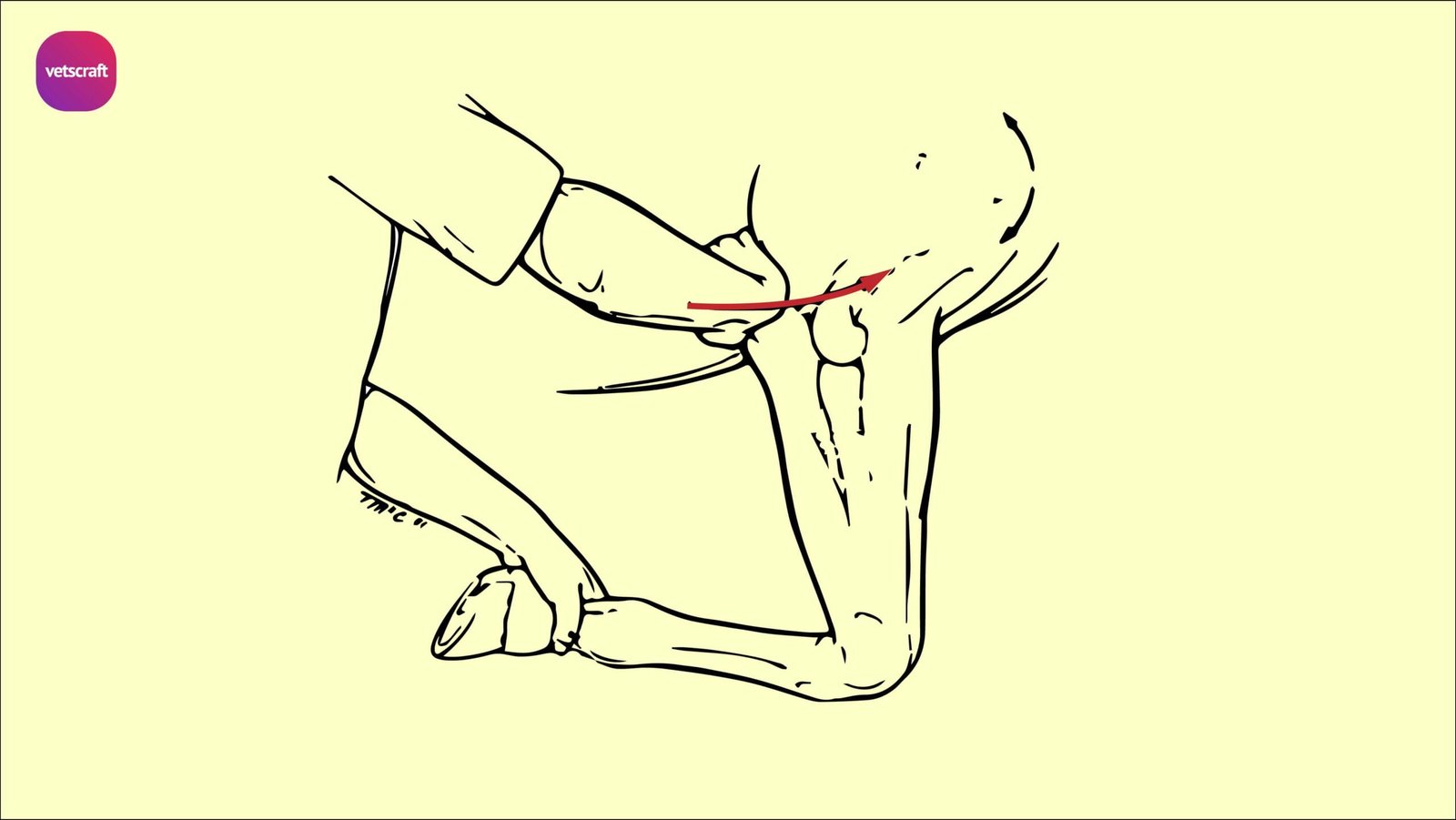
- Manipulation of the elbow into hyperextension may stress the biceps brachii tendon, helping to localize the lesion
- If the localizing signs are not obvious, bursitis is confirmed by centesis and local anesthesia of the bursa. A proximal approach to the bursa is considered to be the most successful for bursal centesis.
- Addition of contrast material and radiographic exam may be necessary to assess the success of centesis.
Treatment
Conservative treatment
- Rest
- Parenteral and/or topical application of NSAID’s
- Intra-synovial injection of bursa with corticosteroids and HA
Surgical treatment
Bursitis that results from a displaced fracture, from osseous changes associated with the proximocranial aspect of the humerus, or from sepsis generally requires surgery to resolve the problem. Incisional as well as arthroscopic approaches to the intertubercular bursa have been used and described.
If a fracture is present the fragment is removed and the bed debrided and smoothed.
Controlled exercise as described for the conservative approach is begun at the time of suture removal in most cases.
In the rare event of calcification of the bicipital tendon, surgical removal of the calcific mass may be attempted.
In cases in which infection appears to be the cause, centesis of the bursa should be done to collect fluid for culture and cytology. Next, the bursa should be drained and then debrided and lavaged copiously under arthroscopic guidance followed by instillation of a broad spectrum antimicrobial into the synovial cavity.
Parenteral administrations of broad-spectrum antibiotics and NSAIDs are required.
In some cases the bursa is left open to drain and heal by second intention. Antimicrobial therapy is generally prolonged, lasting 3 to 4 weeks.
Controlled exercise and moving the affected limb through a passive range of motion is advocated to reduce restrictive adhesion formation.
Prognosis
Acute cases of nonseptic bursitis when a fracture is not the cause often respond favourably to conservative treatment.
Conservative therapy for more chronic cases of nonseptic or septic bursitis appears less satisfactory.
In chronic septic bursitis cases treated conservatively the prognosis appears poor for return to performance unless surgery is performed. Surgical intervention with debridement, lavage, and appropriate antimicrobial therapy and rest gives a favourable prognosis.